Week 2 Pregnancy: Ovulation, Fertile Window, and What to Expect
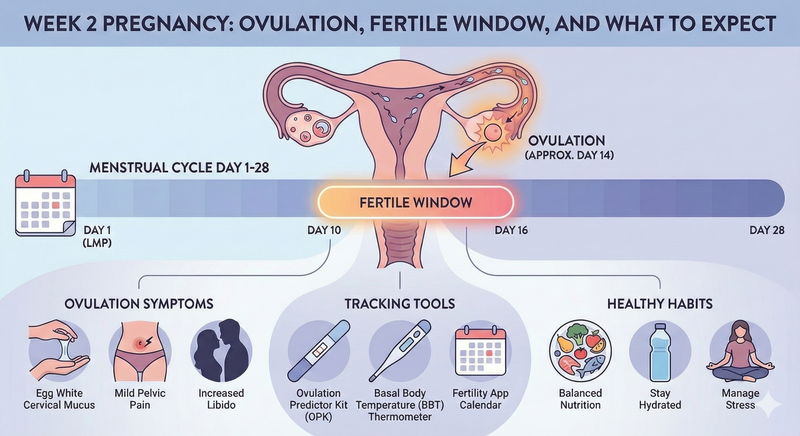
Learn what happens in Week 2 of pregnancy, including ovulation, fertile window timing, body changes, conception chances, and care tips to prepare for pregnancy.
The clinical designation of the second week of pregnancy within the standard obstetric timeline represents a significant departure from biological reality, functioning as a chronometric paradigm rather than an embryological one. Within the traditional 40-week gestational model, the first two weeks typically encompass the follicular phase of the menstrual cycle, a period during which the subject is not yet biologically pregnant. The estimation of the due date traditionally relies on the first day of the last menstrual period, a method that captures the preparatory phase required for successful conception. Consequently, week two is characterized by an intricate orchestration of hormonal signals, cellular maturation, and physiological synchronization that establishes the foundation for all subsequent fetal development.
For a comprehensive look at the preceding stage, see the(week 1 pregnancy guide).
The Chronometric Paradox of Pregnancy Dating
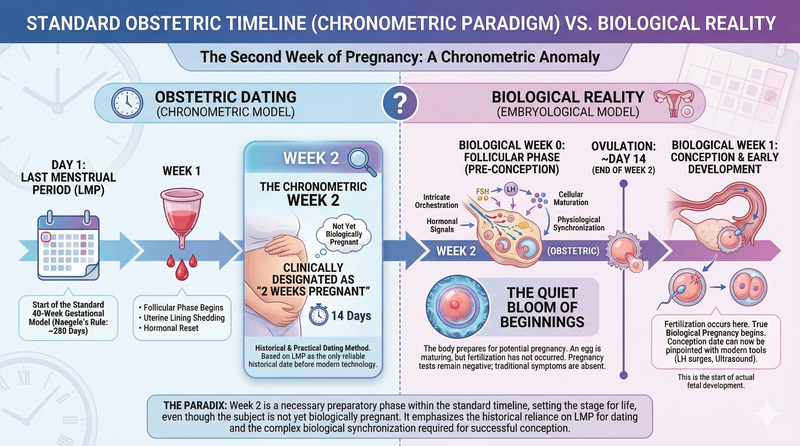
The methodology for calculating pregnancy duration, primarily established through Naegele’s Rule, posits that a full-term pregnancy lasts approximately 280 days from the onset of the last menstrual period. This calculation includes the follicular phase, which typically lasts about 14 days in a standard 28-day cycle. Under this system, "week two" is the interval leading up to ovulation.
The paradox lies in the fact that while a medical professional may classify a patient as being two weeks pregnant, the biological event of fertilization has not yet occurred. This period is best described as the "quiet bloom of beginnings," where the body is preparing the stage—an egg is maturing, ready to meet its match, but the actual state of pregnancy remains a future potentiality [Image 1, Image 3]. Understanding this timeline is essential for patients, as it clarifies why home pregnancy tests remain negative during this interval and why traditional pregnancy symptoms are absent.
Gestational Stages and Biological Progress:
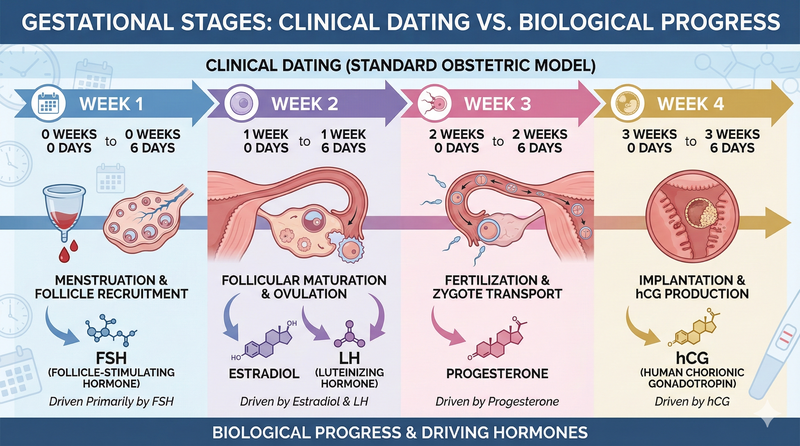
- Week 1: Menstruation and follicle recruitment. This stage is driven primarily by follicle-stimulating hormone (FSH). Clinical dating ranges from 0 weeks 0 days to 0 weeks 6 days.5
- Week 2: Follicular maturation and ovulation. Driven by estradiol and LH. Clinical dating ranges from 1 week 0 days to 1 week 6 days.6
- Week 3: Fertilization and zygote transport. Driven by progesterone. Clinical dating ranges from 2 weeks 0 days to 2 weeks 6 days.8
- Week 4: Implantation and human chorionic gonadotropin (hCG) production. Driven by hCG. Clinical dating ranges from 3 weeks 0 days to 3 weeks 6 days.5
The Endocrinology of the Hypothalamic-Pituitary-Gonadal Axis
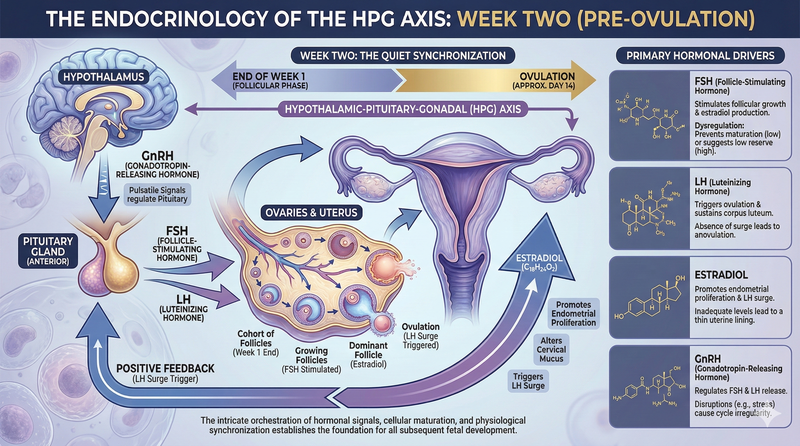
The physiological events of week two are driven by the Hypothalamic-Pituitary-Gonadal (HPG) axis, a complex endocrine circuit responsible for regulating reproductive function.10 This axis operates through a series of pulsatile signals and feedback loops that ensure the timely maturation and release of a viable oocyte. The process begins in the hypothalamus with the release of Gonadotropin-Releasing Hormone (GnRH).
During the transition into week two, FSH levels rise, signaling the ovaries to promote the growth of a cohort of follicles.9 As these follicles grow, they secrete increasing amounts of estradiol . This rise in estrogen serves several critical functions: it thickens the endometrial lining, alters the consistency of cervical mucus, and eventually triggers the LH surge required for ovulation.9 The "behind the scenes" work of LH and FSH is a quiet synchronization that prepares the body for the fertile window .
Primary Hormonal Drivers:
- FSH (Follicle-Stimulating Hormone): Stimulates follicular growth and estradiol production.9 Dysregulation can prevent egg maturation (low levels) or suggest low reserve (high levels).12
- LH (Luteinizing Hormone): Triggers ovulation and sustains the corpus luteum.11 An absence of the surge leads to anovulation.10
- Estradiol: Promotes endometrial proliferation and the LH surge.9 Inadequate levels lead to a thin uterine lining.13
- GnRH (Gonadotropin-Releasing Hormone): Regulates the release of FSH and LH from the pituitary.11 Disruptions can be caused by stress, leading to cycle irregularity.14
Endometrial Dynamics: Preparing the Stage
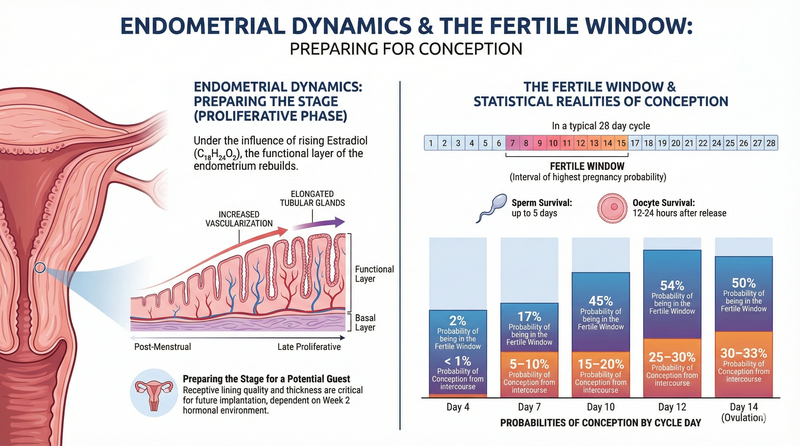
While the ovaries focus on the egg, the uterus undergoes the proliferative phase of the menstrual cycle. Under the influence of rising estradiol, the functional layer of the endometrium begins to rebuild.2 The tissue becomes increasingly vascularized, and the uterine glands become more tubular and elongated. This preparation is described as "preparing the stage" for a potential guest [Image 3].
The quality of the endometrium is a critical factor in successful implantation. A receptive lining must reach a certain thickness to support the attachment of a blastocyst.14 Although implantation will not occur for another 7 to 10 days, the success of that event is entirely dependent on the hormonal environment established during week two.2
The Fertile Window and Statistical Realities of Conception
The fertile window is the interval during which intercourse has the highest probability of resulting in pregnancy. Biologically, this window is defined by the lifespan of the gametes: the oocyte survives for only 12 to 24 hours after release, whereas healthy sperm can survive within the female reproductive tract for up to five days.8
Probabilities of Conception by Cycle Day:
- Day 4: 2% probability of being in the fertile window; < 1% probability of conception from intercourse.15
- Day 7: 17% probability of being in the fertile window; 5–10% probability of conception from intercourse.1
- Day 10: 45% probability of being in the fertile window; 15–20% probability of conception from intercourse.15
- Day 12: 54% probability of being in the fertile window; 25–30% probability of conception from intercourse.1
- Day 14: 50% probability of being in the fertile window; 30–33% probability of conception from intercourse.16
Nutritional Foundations and Lifestyle Support
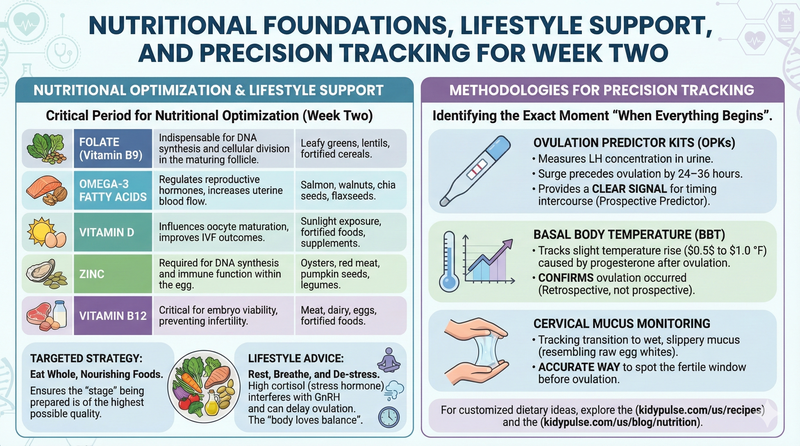
The second week of pregnancy is a critical period for nutritional optimization. A balanced diet rich in plant-based proteins, healthy fats, and antioxidants has been shown to improve fertility outcomes.14 For customized dietary ideas, explore the(https://kidypulse.com/us/recipes) and the(https://kidypulse.com/us/blog/nutrition).
Key Micronutrients for Week Two:
- Folate (Vitamin B9): Indispensable for DNA synthesis and cellular division in the maturing follicle.5 Sources: leafy greens, lentils, and fortified cereals.
- Omega-3 Fatty Acids: Regulates reproductive hormones and increases blood flow to the uterus.18 Sources: salmon, walnuts, chia seeds, and flaxseeds.
- Vitamin D: Influences oocyte maturation and IVF outcomes.5
- Zinc: Required for DNA synthesis and immune function within the egg.5
- Vitamin B12: Critical for embryo viability and preventing infertility.5
The instruction to "eat whole, nourishing foods" is a targeted strategy to ensure the "stage" being prepared is of the highest possible quality [Image 5]. Additionally, managing stress is vital, as high levels of cortisol can interfere with the pulsatile release of GnRH, potentially delaying ovulation.14 Recommendations often include "rest, breathe, and de-stress," as the "body loves balance" [Image 5].
Methodologies for Precision Tracking
For many, identifying the exact moment "when everything begins" is a priority [Image 2]. Several methods exist to track the events of week two:
- Ovulation Predictor Kits (OPKs): These measure the concentration of LH in the urine. Because the surge precedes ovulation by 24–36 hours, it provides a clear signal for timing intercourse.1
- Basal Body Temperature (BBT): BBT tracks the slight rise in temperature ($0.5$ to $1.0$ °F) caused by progesterone after ovulation.19 It confirms ovulation occurred but is not a prospective predictor.4
- Cervical Mucus Monitoring: Tracking the transition to wet, slippery mucus (resembling raw egg whites) is an accurate way to spot the fertile window before ovulation.8
Myth vs Truth: Physical Sensations
A common myth is that people can "feel" the pregnancy beginning in week two. The truth is that the body is simply getting ready; any symptoms felt are typically related to ovulation, as hCG is not yet present [Image 6]. Symptoms may include Mittelschmerz (ovulation pain), breast tenderness, or a heightened sense of smell.4

Comments
No comments yet. Be the first to leave a comment!